[ad_1]
The unwinding of pandemic enrollment protections in Medicaid helped accelerate states’ expansion of eligibility for key groups and adoption of policy and system changes to streamline renewal processes for enrollees, according to findings from a new KFF survey of state Medicaid officials. These changes mean that the return to “routine” operations when the unwinding period ends will not be a return to pre-pandemic operations in many states.
The survey examined actions states have taken to enhance systems, processes, and communications, as well as key state Medicaid eligibility, enrollment, and renewal policies and procedures in place for children and most non-elderly adults as of May 2024.
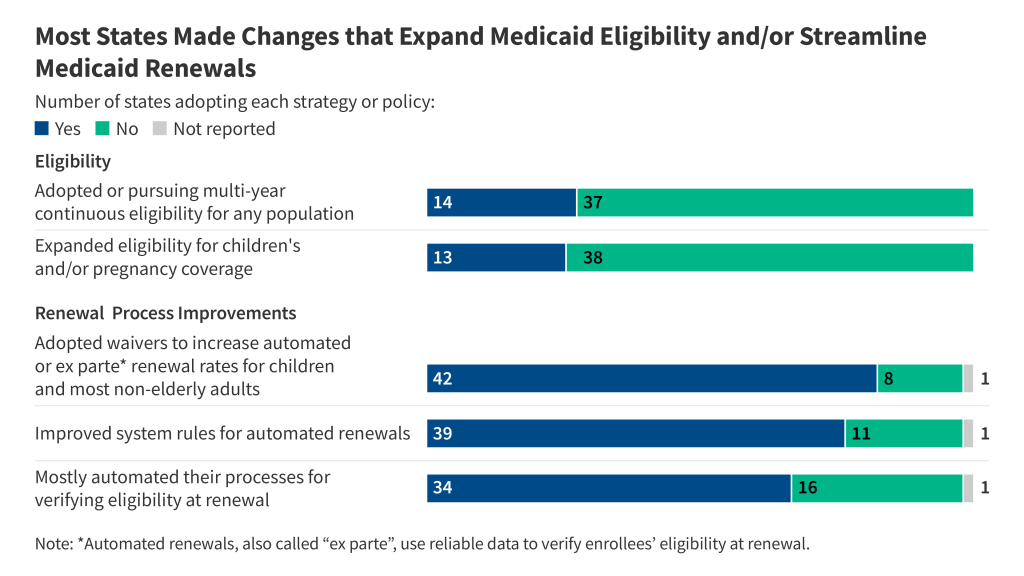
States report changes in the following key areas:
Coverage for children and pregnant individuals: Several states are taking steps to expand coverage for children and pregnant individuals. In 2024, five states increased eligibility levels for children and/or pregnancy coverage and eight states extended coverage to certain immigrant children and/or pregnant individuals. Eighteen states have eligibility levels above the median for both children (255% FPL) and pregnancy (210% FPL). Building on the experience of continuous enrollment during the pandemic, 13 states are seeking to keep children continuously enrolled in Medicaid for more than a year.
Automated renewal processes: All states reported taking actions to increase automated renewal rates during the unwinding. Through automated renewals, also called “ex parte” renewals, Medicaid eligibility workers use reliable data to verify enrollees’ eligibility at renewal. This approach decreases paperwork for enrollees and states as well as gaps in coverage. Forty-two states adopted waiver flexibilities to increase automated renewal rates, such as allowing automated renewals for people without income or using eligibility for other income-based assistance programs to confirm Medicaid eligibility.
Other changes: In addition to improving automated processes, ten states say they simplified renewal forms, and seven states extended the time enrollees have to respond to renewal notices. States have also boosted direct outreach to enrollees through multiple modes, including text, email, and automated calls, and 37 states plan to maintain the enhanced outreach.
Despite these changes, states encountered numerous obstacles to simplifying renewals for enrollees during the unwinding period, including workforce issues and problems with their eligibility systems. Most states (41) reported frontline eligibility staff vacancies, and 32 of these states identified the impact of the vacancies as significant or moderate.
A companion KFF Medicaid survey examining eligibility, enrollment, and renewal policies for seniors and people with disabilities found eligibility policies for these populations vary across states, but states made similarly wide-ranging changes to streamline renewal processes for these enrollees. Other key takeaways include:
- Application processes for seniors and people with disabilities: Most states (38) now use the same processes to determine income eligibility for all Medicaid enrollees, but the need to document assets may make applications more onerous for seniors and people with disabilities. All states but California require many in this group to demonstrate that their assets are below Medicaid eligibility limits, and asset eligibility processes are often more cumbersome than the process for income.
- Renewal policies for seniors and people with disabilities: Renewal policies for seniors and people with disabilities increasingly resemble those for other populations. All responding states only renew eligibility annually for seniors and people with disabilities, and 47 states provide enrollees with 30 days to return renewal information and a 90-day reconsideration period following a procedural disenrollment.
The 22nd annual survey of state Medicaid and CHIP programs officials was conducted by KFF and the Georgetown University Center for Children and Families in March 2024. The KFF Survey of Medicaid Financial Eligibility & Enrollment Policies for Seniors & People with Disabilities was also conducted in March 2024 by KFF and Watts Health Policy Consulting. Overall, 49 states and the District of Columbia responded to both surveys, although response rates for specific questions varied. (Florida was the only state that did not respond.)
[ad_2]
Source link

