[ad_1]
Social determinants of fitness (SDOH) are the stipulations through which individuals are born, develop, reside, paintings and age. Whilst there are limits, states can use Medicaid – which, through design, serves a essentially low-income inhabitants with larger social wishes – to handle social determinants of fitness. To enlarge alternatives for states to make use of Medicaid to handle health-related social wishes, The Facilities for Medicare & Medicaid Services and products or CMS announced new flexibilities to be had to states to via managed care and thru Section 1115 demonstration waivers. New CMS steerage accompanies the Biden-Harris Management’s free up of the U.S. Playbook to Address Social Determinants of Health and HHS’s Call to Action to Address Health-Related Social Needs. Whilst fitness techniques like Medicaid can play a supporting function, CMS stresses the brand new HRSN projects don’t seem to be designed to interchange different federal, state, and native social provider techniques however fairly to enrich and coordinate with those efforts. The sources equipped to this point via Medicaid are reasonably modest compared to the social wishes that exist. This temporary outlines the variety of Medicaid government and flexibilities that can be utilized so as to add advantages and design techniques to handle the social determinants of fitness (Determine 1).
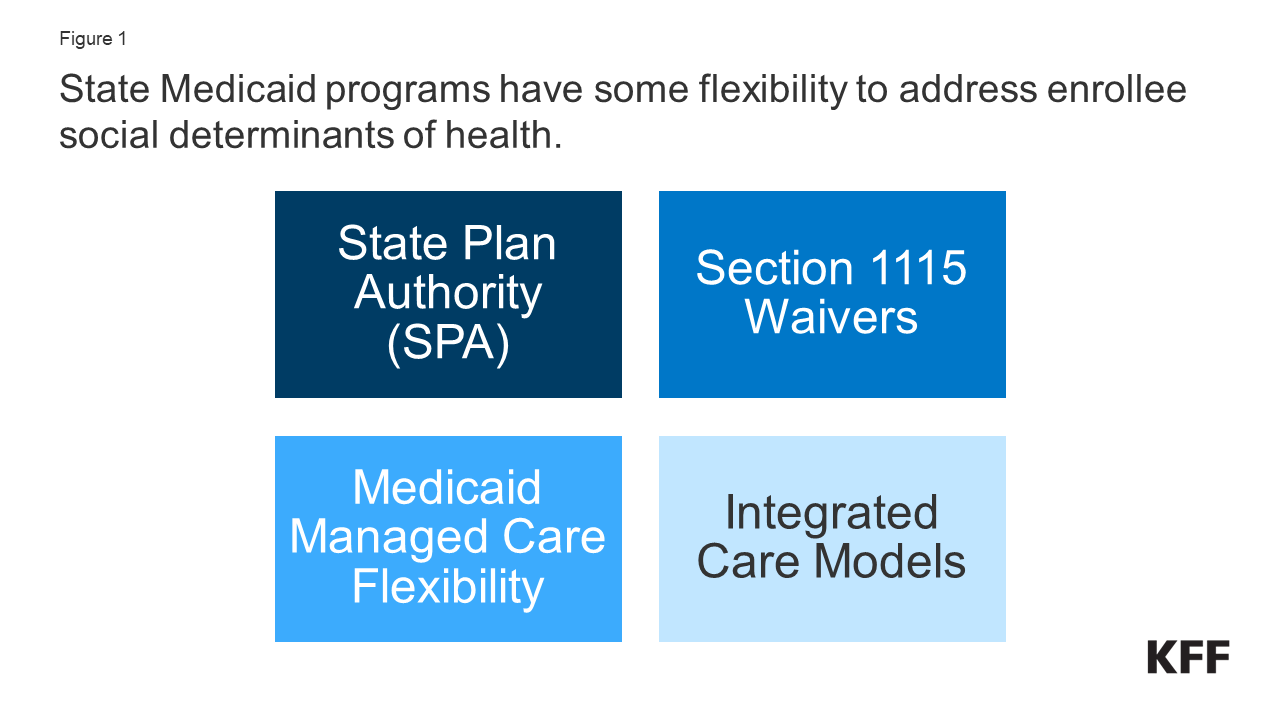
Determine 1: State Medicaid techniques have some flexibility to handle enrollee social determinants of fitness.
What Are Social Determinants of Well being?
Social determinants of fitness are the stipulations through which individuals are born, develop, reside, paintings and age. They come with components like financial balance, schooling, group and bodily surroundings, employment, and social enhance networks, in addition to get entry to to fitness care (Determine 2).
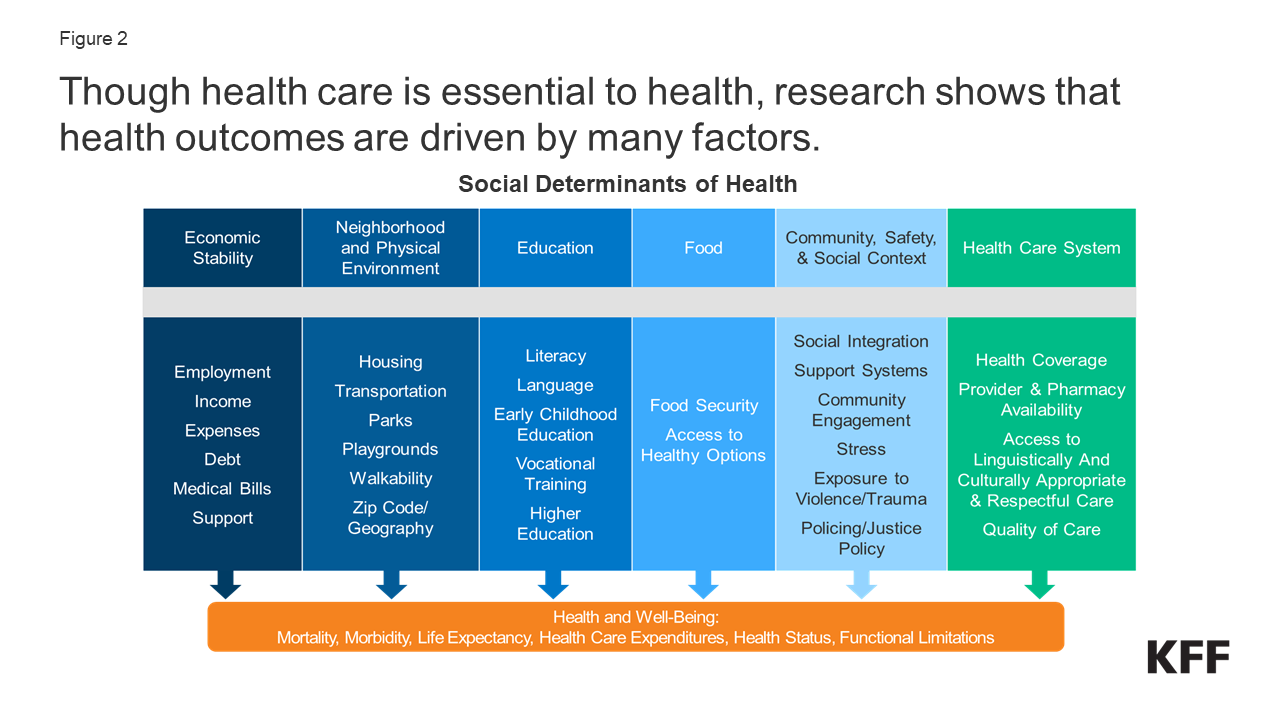
Determine 2: Although fitness care is very important to fitness, analysis presentations that fitness results are pushed through many components.
Although fitness care – and, through extension, fitness protection – is very important to fitness, analysis presentations that fitness results are pushed through an array of things, together with underlying genetics, fitness behaviors, social, financial, and environmental components. Whilst there may be these days no consensus within the analysis at the magnitude of the relative contributions of each and every of those components to fitness, research recommend that fitness behaviors and social and financial components are number one drivers of fitness results, and social, and financial components can form folks’ fitness behaviors. There’s intensive analysis that concludes that addressing social determinants of fitness is vital for making improvements to fitness results and lowering fitness disparities.
Each fitness and non-health sectors were engaged in projects to handle social determinants of fitness. Out of doors of the fitness care gadget, non-health sector projects search to form insurance policies and practices in ways in which advertise fitness and fitness fairness. Throughout the fitness care sector, a huge vary of projects were introduced on the federal, state, and native ranges and through plans and suppliers to handle social determinants of fitness, together with efforts inside of Medicaid.
How Can Medicaid be Used to Deal with Social Determinants of Well being?
State Medicaid techniques can upload sure non-clinical services and products to domestic and community-based services and products (HCBS) techniques to enhance seniors and folks with disabilities. Most often, states have now not been ready to make use of federal Medicaid finances to pay the direct prices of non-medical services and products like housing and meals. Alternatively, inside of Medicaid, states can use a variety of state plan and waiver government (e.g., 1905(a), 1915(i), 1915(c), or Segment 1115) so as to add sure non-clinical services and products to the Medicaid get advantages bundle together with case control, housing helps, employment helps, and peer enhance services and products. Traditionally, non-medical services and products were incorporated as a part of Medicaid domestic and community-based services and products techniques for individuals who want assist with self-care or family actions because of incapacity or power sickness.
Out of doors of Medicaid HCBS government, state Medicaid techniques have traditionally had extra restricted flexibility to handle social determinants of fitness. Positive choices exist beneath Medicaid state plan authority in addition to Segment 1115 authority so as to add non-clinical advantages. Moreover, beneath federal Medicaid controlled care regulations, controlled care plans have some flexibility to pay for non-medical services and products. Different Medicaid cost and supply gadget reforms, just like the formation of Responsible Care Organizations (ACOs), might supply flexibility or alternatives to hide non-medical services and products that enhance fitness as neatly.
To enlarge alternatives for states to make use of Medicaid to handle health-related social wishes, CMS announced new flexibilities to be had to states via Medicaid managed care authority and thru Section 1115 demonstration waivers. CMS defines health-related social wishes (or “HRSN”) as a person’s unmet, antagonistic social stipulations (e.g., housing instability, homelessness, diet lack of confidence) that give a contribution to deficient fitness and are a results of underlying social determinants of fitness. New CMS steerage builds on guidance launched in 2021. The rest sections define the principle Medicaid government and flexibilities that can be utilized so as to add advantages and design techniques to handle the social determinants of fitness past HCBS techniques. Some efforts might cope with a unmarried factor (e.g., housing, or meals safety) whilst different efforts and projects are designed to handle a variety of social determinants of fitness.
Medicaid Controlled Care Plan Authority
With over two-thirds of Medicaid beneficiaries enrolled in complete, risk-based managed care plans nationally, fitness plans can also be a very powerful a part of efforts to handle enrollee social determinants of fitness. States pay Medicaid controlled care organizations (MCOs) a collection in line with member per thirty days cost for the Medicaid services and products specified of their contracts. Capitation charges supply prematurely mounted bills to plans for anticipated usage of coated services and products, management prices, and benefit.
Below federal Medicaid controlled care regulations, Medicaid MCOs can also be given flexibility to pay for non-medical services and products via “in-lieu-of” authority. States might permit Medicaid MCOs the choice to provide (and supply beneficiaries the strategy to obtain) services and products or settings that exchange for same old Medicaid advantages (known as “in lieu of” services and products (or “ILOS”)) if the synthetic provider is medically suitable and cost-effective. For instance, a state may just authorize in-home prenatal visits for at-risk pregnant beneficiaries as an alternative choice to conventional workplace visits or services and products equipped through peer helps, as an alternative choice to psychosocial rehabilitation services and products for individuals with behavioral fitness wishes. The prices of the ILOS are constructed into controlled care charges. In January 2023, CMS launched steerage that paves the way in which for states to permit Medicaid MCOs to provide services and products, like housing and diet helps, as substitutes for same old Medicaid advantages. The brand new steerage establishes monetary guardrails and new necessities for ILOS and clarifies those exchange services and products can also be preventive in nature as an alternative of a right away exchange (e.g., offering a dehumidifier to a person with bronchial asthma ahead of emergency care is wanted). This steerage follows the approval of a California proposal to make use of ILOS. In Would possibly 2023, the Biden management issued a proposed rule associated with controlled care get entry to, finance, and high quality. Within the proposed rule, CMS seeks to codify its January 2023 ILOS steerage. KFF’s 2023 survey of state Medicaid directors discovered few states accepted MCOs to hide SDOH-related services and products (e.g., housing, meals, or different) as ILOS as of July 2023.
Below federal regulations, Medicaid MCOs will pay for non-medical services and products as “value-added” services and products. “Worth-added” services and products are additional services and products MCOs voluntarily supply out of doors of coated contract services and products. Those services and products can’t be constructed into controlled care charges. Examples come with secure drowsing areas for babies, maintenance and cleansing services and products to cut back bronchial asthma triggers, set up of a bath grasp bar, and fitness play and workout techniques.
States might put into effect MCO procurement and contracting methods, together with high quality necessities connected to SDOH. In a 2023 KFF survey of Medicaid directors, maximum MCO states reported leveraging Medicaid MCO contracts to advertise no less than one approach to cope with social determinants of fitness in FY 2023 (Determine 3). Greater than part of MCO states reported requiring MCOs to display enrollees for social wishes, display enrollees for behavioral fitness wishes, supply referrals to social services and products, and spouse with community-based organizations (CBOs). Fewer states reported requiring MCO network reinvestment (i.e., directing plans to reinvest a portion of income or income into the communities they serve) in comparison to different methods. States can use incentive bills or high quality withhold preparations to praise plans for investments and/or enhancements in SDOH. For instance, states might supply incentive bills to plans that display enrollees for social wishes or make different strategic investments in addressing health-related social wishes or incentive bills to give a boost to or deal with high quality whilst reducing prices. Moreover, many plans have advanced projects and engaged in actions to handle enrollees’ social wishes past state necessities; alternatively, it’s tough to assemble nationwide information to replicate this.
Within the Institute for Medicaid Innovation’s 2023 Medicaid managed care survey, plans indicated state Medicaid businesses may just enhance MCO efforts to handle enrollee social wishes through making improvements to information sharing (e.g., between the state and MCOs and between govt businesses), expanding monetary sources (together with to enhance the facilitation of partnerships and new cost fashions), and facilitating contracting with CBOs.
States can direct controlled care plans to make bills to their community suppliers to additional state objectives and priorities, together with the ones associated with addressing social determinants of fitness. States can search CMS approval to require MCOs to put into effect value-based buying fashions for supplier compensation (e.g., pay for efficiency, bundled bills) or take part in multi-payer or Medicaid-specific supply gadget reform or efficiency growth projects. For instance, a state might require controlled care plans to put into effect selection cost fashions (APMs) or incentive bills to inspire suppliers to display for socioeconomic threat components.
Segment 1115 Waivers
Via Section 1115 authority, states can take a look at approaches for addressing SDOH together with asking for federal matching finances to check SDOH connected services and products and helps in ways in which advertise Medicaid program targets. Segment 1115 waivers typically replicate priorities recognized through states and CMS, in addition to converting priorities from one presidential management to any other. Whilst now not required through statute, longstanding coverage calls for that Segment 1115 waivers be finances impartial for the government. As defined in CMS’s 2021 guidance, states can request federal matching finances via Segment 1115 to check the effectiveness of offering SDOH-related services and products and helps. States too can take a look at selection cost methodologies designed to handle SDOH beneath Segment 1115 authority. Previous to the Biden management announcement of recent HRSN waiver flexibilities (mentioned in additional element beneath), a number of states had authorized Segment 1115 waivers that aimed to handle enrollee social determinants of fitness. Those SDOH waivers have been typically slender in scope (services and products and goal populations) or pilot techniques concentrated on particular areas. For instance, in October 2018, CMS authorized North Carolina’s Wholesome Alternatives Pilots that function in 3 geographic areas of the state and supply services and products to handle enrollee wishes associated with housing, meals, transportation, and interpersonal protection. Some waivers allowed MCOs or ACOs flexibility to provide health-related services and products however stopped in need of requiring them to take action.
In December 2022, CMS introduced a Segment 1115 demonstration waiver opportunity to enlarge the equipment to be had to states to handle HRSN. In November 2023, CMS issued an in depth Medicaid and CHIP HRSN Framework accompanied through an Informational Bulletin (CIB). HRSN services and products that will likely be regarded as beneath the brand new framework come with housing helps, diet helps, and HRSN case control (and different services and products on a case-by-case foundation) (Determine 4). As of January 2024, CMS has authorized Segment 1115 demonstrations in 8 states (Arizona, Arkansas, California, Massachusetts, New Jersey, New York, Oregon, and Washington) that authorize evidence-based HRSN services for particular high-need populations. Approvals come with protection of hire/transient housing and utilities for as much as 6 months and meal enhance as much as 3 foods in line with day (as much as 6 months). HRSN services and products will have to be medically suitable (the use of state-defined medical and social threat components) and voluntary for enrollees. States can upload HRSN services and products to the convenience bundle and might require controlled care plans to provide the services and products to enrollees who meet state standards. Federal expenditures also are to be had to construct the capability of network founded HRSN suppliers that can require technical help and infrastructure enhance to turn out to be Medicaid suppliers. Moreover, the Biden management has expressed enhance for “community care hubs” (or an identical fashions) that target aligning fitness and social care and might facilitate care coordination in addition to increase, organize, and enhance a community of CBOs.
CMS steerage specifies spending for HRSN can’t exceed 3% of general annual Medicaid spend. CMS signifies HRSN spending is not going to require offsetting financial savings (that can another way be required for services and products licensed/financed beneath Segment 1115). State spending on connected social services and products (ahead of the waiver) will have to be maintained or larger. To give a boost to get entry to, states will have to additionally meet minimal supplier cost fee necessities for number one care, behavioral fitness, and obstetrics services and products. HRSN services and products are topic to tracking and analysis necessities, together with reporting on high quality and fitness fairness measures. In November 2023, HHS and HUD announced the release of a brand new finding out collaborative that can enhance states with the implementation of Segment 1115 housing-related helps, together with serving to states give a boost to collaboration and coordination between organizations and programs that offer housing services and products.
State Plan Authority & Supply Device Reform Fashions
States might elect to incorporate not obligatory advantages that cope with social determinants beneath Segment 1905(a) State Plan authority. For instance, states might come with rehabilitative services and products, together with peer helps and/or case control (or “centered” case control) services and products, beneath their Medicaid state plan. States that make a selection to provide those services and products regularly goal services and products in keeping with fitness or useful want standards. Peer helps can assist folks coordinate care and social helps and services and products, facilitating linkages to housing, transportation, employment, diet services and products, and different community-based helps. Case control services and products too can lend a hand folks in having access to clinical, social, instructional, and different services and products. Case control services and products are regularly a very powerful part of HCBS techniques however may also be used to handle a broader vary of enrollee wishes.
States can give broader services and products to enhance fitness in the course of the not obligatory fitness domestic state plan get advantages possibility established through the ACA. Below this feature (Segment 1945), states can identify fitness properties to coordinate deal with individuals who have power stipulations. Well being domestic services and products come with complete care control, care coordination, fitness promotion, complete transitional care, affected person and circle of relatives enhance, in addition to referrals to network and social enhance services and products (equivalent to housing, transportation, employment, or dietary services and products). States obtain a 90% federal fit fee for certified fitness domestic provider expenditures for the primary 8 quarters beneath each and every fitness domestic., A federally funded analysis of the Well being Properties type discovered that the majority suppliers reported vital enlargement of their skill to attach sufferers to nonclinical social services and products and helps beneath the type, however that loss of strong housing and transportation have been not unusual issues for plenty of enrollees that have been tough for suppliers to handle with inadequate reasonably priced housing and hire enhance sources.
Built-in care fashions, together with patient-centered clinical domestic (PMCHs) and Responsible Care Organizations (ACOs), incessantly emphasize person-centered, complete care and most often contain partnerships with community-based organizations and social services and products businesses. Built-in care fashions would possibly cope with social determinants of fitness via interdisciplinary care groups or care coordination services and products. Fee mechanisms tied to those fashions (e.g., in line with member per thirty days bills (without or with high quality or charge incentives) or shared financial savings/threat fashions with high quality necessities) might supply incentives for suppliers to handle the huge wishes of Medicaid beneficiaries.
Having a look Forward
Whilst fitness techniques like Medicaid can play a supporting function, steerage from CMS stresses the brand new HRSN projects don’t seem to be designed to interchange different federal, state, and native social provider techniques however fairly to enrich and coordinate with those efforts. The sources equipped via Medicaid to handle social determinants of fitness are reasonably modest within the face of the social wishes that exist, and there may be ongoing debate over how successfully the fitness care gadget can meet those wishes.
Spaces to look at come with which health-related services and products states might acquire approval to combine beneath controlled care authority and/or Section 1115, how states outline goal populations, and the way CMS and states negotiate finances neutrality phrases (a subject matter that Republican individuals of the United States Space Power and Trade have raised concerns about).
States that experience now not pursued however is also excited about new HRSN flexibilities can be told from the implementation revel in of early adopters, together with how states and plans paintings with community-based organizations and coordinate with federal, state, and native social provider techniques. Whilst there may be some proof, ,,,, ILOS and Segment 1115 tracking and analysis reviews might yield new information involving how addressing sure enrollee social wishes might have an effect on fitness care usage, spending, and fitness results. In the end, whether or not states can maintain investment streams for HRSN long run and the way long term adjustments in Management might impact states’ skill to pursue those projects via waivers will likely be vital to look at.
[ad_2]
Source link
